
For many ophthalmologists, the management of astigmatism is one of the most common rate-limiting steps that prevents patients from achieving optimal quality of vision and satisfaction after refractive cataract surgery. Residual astigmatism of 0.50 D after cataract surgery and sometimes less may result in glare, symptomatic blur, ghosting, and halos. In a study of 4,540 eyes, corneal astigmatism was present in the majority of patients undergoing cataract surgery, with at least 1.50 D measured in 22.2% of study eyes.1 Approximately 38% of eyes undergoing cataract surgery have at least 1.00 D of preexisting corneal astigmatism, while 72% of patients have 0.50 D or more.2 Surgeons can reduce astigmatism with photoablation using an excimer laser, toric IOLs, and femtosecond laser arcuate incisions. Additionally, limbal relaxing incisions (LRIs) are a valid alternative or adjunctive therapy (Figure 1). Although the use of manual LRIs has been an art form with inherent surgeon variability and predictability and although LRIs require expertise, there is enormous value to using this technique for today's cataract surgery patients.
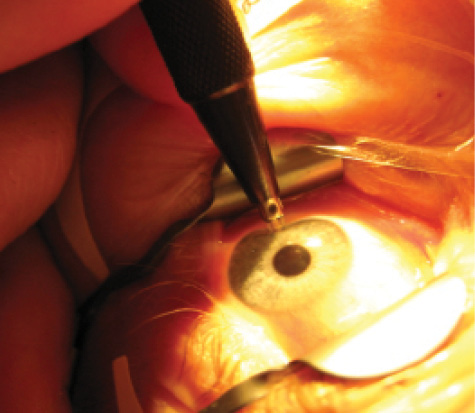
Figure 1. LRIs for preexisting astigmatism can be easily performed in the OR.
COST-EFFECTIVE ALTERNATIVE FOR SMALL REFRACTiVE ERRORS
I have found that most patients tolerate postoperative astigmatism of 0.50 D or less. New incisional technologies such as the femtosecond laser offer greater predictability and a repeatable incision depth, and laser arcs can be more centrally located compared to LRIs3; however, patients and surgeons should evaluate the cost-effectiveness of a manual LRI, which is certainly a better alternative to no treatment at all. At my practice, we extensively use laser arcuate incisions and toric IOLs but have found a significant role for manual LRIs.
There is a myth in the refractive surgery world that IOL patients will tolerate small refractive errors. Nothing could be further from the truth. All cataract surgery patients—particularly those receiving presbyopia-correcting IOLs—are incredibly sensitive to even minor cylindrical errors. Refractive IOL surgeons must be willing and able to treat postoperative astigmatism to achieve happy postoperative patients. Again, based on my experience, patients will tolerate 0.50 D of cylinder or less. My goal as a refractive cataract surgeon, however, is not merely to give patients vision they will tolerate, but to exceed their expectations. For this reason, I often fine-tune good results in cataract patients with even 0.50 D of residual cylinder. When patients have residual refractive error after cataract surgery, I always attempt to expedite treatment as soon as it is safe for them. LRIs can usually be performed as early as 2 weeks postoperatively.
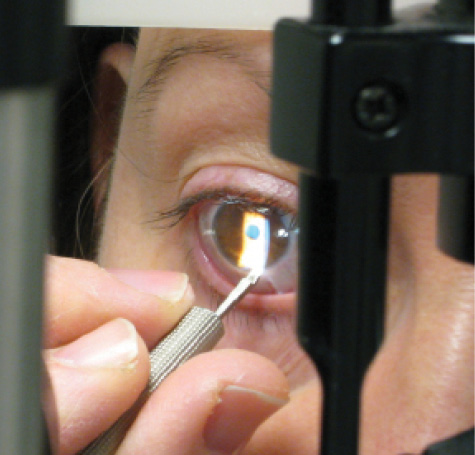
Figure 2. LRIs can be performed at the slit lamp in the office.
MY METHOD
For the past several years, I have used a preset diamond knife that has a 15º tip angulation, making it ideal for use at the slit lamp as well as in the OR. For the slit-lamp procedure (Figure 2), I use lidocaine gel to anesthetize the eye. I use a phoropter to confirm the incision axis, and I operate on this axis exactly as I would under an operating microscope. I make certain that the patient's head is forward, as I come from the side, making one incision to achieve 0.50 to 0.75 D of correction. After this 30-second procedure, patients walk away seeing better that day.
At a Glance
• Manual LRIs are a cost-effective alternative to photoablation
with an excimer laser, toric IOLs, and
femtosecond laser arcuate incisions.
• LRIs can be performed as early as 2 weeks
postoperatively.
• Surgeons should practice the basic techniques for placing
LRIs and eventually develop their own nomograms
to achieve consistent results.
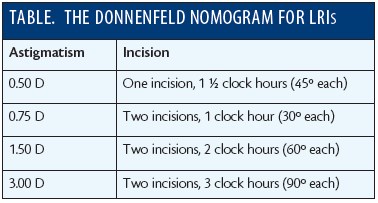
NOMOGRAMS FOR SMALL AMOUNTS OF CYLINDER
Notable surgeons such as Louis “Skip” D. Nichamin, MD4; Douglas Koch, MD5; and James Gills, MD,6 have proposed different nomograms for correcting small amounts of cylinder with LRIs. Although these formulae are meant to simplify the placement of the incisions, their specific adjustments for age and axis cylinder can give the impression that the procedure is overly complex, precise, and unforgiving. In general, surgeons should practice the basic techniques for placing LRIs and eventually develop their own nomograms to achieve consistent results. The Table outlines the Donnenfeld nomogram for LRIs.
A very useful resource is the website www.lricalculator.com. It provides a vector analysis of the cataract incision to fine-tune astigmatic results and an image that can be brought to the OR. The website uses both the Donnenfeld and Nichamin nomograms.
CONCLUSION
I believe that LRIs are underutilized for correcting primary astigmatism at the time of surgery and postoperative residual astigmatism. Ophthalmologists who successfully transition from cataract to refractive IOL surgery do so because they pay attention to the details that improve their patients' visual outcomes. For many surgeons, this means learning to perform manual LRIs. n
1. Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC, et al. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35:70-75.
2. Hill W. Expected effects of surgically induced astigmatism on AcrySof toric intraocular lens results. J Cataract Refract Surg. 2008;34:364-367.
3. Slade SG. Femtosecond laser arcuate incision astigmatism correction in cataract surgery. Paper presented at: The Cornea Subspecialty Day, ASCRS/ASOA Symposium; March 25, 2011; San Diego, CA.
4. Nichamin LD. Nomogram for limbal relaxing incisions. J Cataract Refract Surg. 2006;32:1048.
5. Wang L, Misra M, Koch DD. Peripheral corneal relaxing incisions combined with cataract surgery. J Cataract Refract Surg. 2003;29:712-722.
6. Gills JP. Treating astigmatism at the time of cataract surgery. Curr Opinion Ophthalmol. 2002;13:2-6.
Eric D. Donnenfeld, MD
• professor of ophthalmology at NYU and a trustee of Dartmouth
Medical School in Hanover, New Hampshire
• (516) 766-2519; ericdonnenfeld@gmail.com


